Executive Summary: Tracking Telehealth Changes State-by-State In Response To COVID-19 - Healthcare - United States - Mondaq | By The Perfect Enemy
To print this article, all you need is to be registered or login on Mondaq.com.
As the COVID-19 pandemic continues across the United States,
states, payers, and providers are looking for ways to expand access
to telehealth services. Telehealth is an essential tool in ensuring
patients are able to access the healthcare services they need in as
safe a manner as possible. In order to provide our clients with
quick and actionable guidance on the evolving telehealth landscape,
Manatt Health has developed a federal and comprehensive 50-state
tracker for policy, regulatory and legal changes related to
telehealth during the COVID-19 pandemic. Below is the executive
summary, which outlines federal developments from the past two
weeks, new state-level developments, and older federal
developments. The full tracker with details for each state is
available through Manatt on Health, Manatt Health’s
premium subscription service. For more information, contact Jared
Augenstein at jaugenstein@manatt.com.
New Federal Developments
| New Item | Activity |
|---|---|
Introduced January 9, 2023 |
|
Passed December 29, 2022 |
|
New State-Level Developments
Note: As indicated in the table below, several states have
recently taken action to update, continue, or renew their state of
emergencies for COVID-19 in response to the rise of new cases
linked with the Omicron variant. These updates are highlighted
below because in many states, temporary telehealth flexibilities
are tied to the status of state of emergency declarations.
| State | Activity |
|---|---|
Delaware |
|
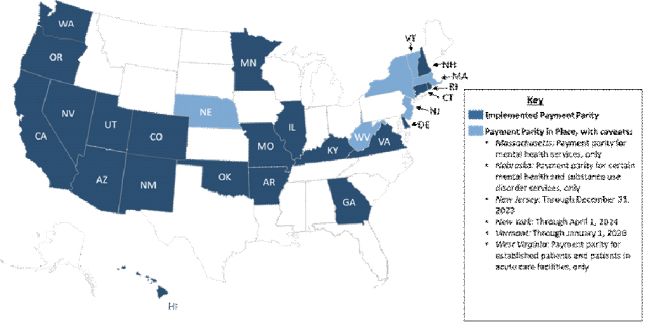
Payment Parity Permanent State Laws and Statutes
Payment Parity requires that health care providers are
reimbursed the same amount for telehealth visits as in-person
visits. During the COVID-19 pandemic, many states implemented
temporary payment parity through the end of the public health
emergency. Now, many states are implementing payment parity on a
permanent basis. As portrayed in Figure 1, as of January 2023, 21
states have implemented policies requiring payment parity, 6 states
have payment parity in place with caveats, and 23 states have no
payment parity.
Figure 1. Map of States With Laws Requiring Insurers to
Implement Payment Parity (as of January 2023)
Federal Developments More than Two Weeks Old
Executive Branch Activity
| Policy | Details |
|---|---|
Released November 7, 2022 |
|
Released November 2, 2022 |
For more information on the Final Rule for the CY 2023 |
Released September 15, 2022 |
|
| Policy | Details |
NIH to Fund Four Telehealth Cancer Centers of Announced August 18, 2022 |
|
Proposed Medicare Physician Fee Schedule for CY Released July 7, 2022 |
|
Issued June 13, 2022 |
|
HHS Announces $16.3 Million to Expand Telehealth Announced May 10, 2022 |
|
Omnibus FY 2022 Spending Bill |
|
In January 2022, CMS released “CARES Act Telehealth |
|
In January 2022, CMS released “Changes in Access to |
|
CY2022 Telehealth Update Medicare Physician Fee Released on Jan. 14, 2022 |
|
On December 6, CMS released updates to the State Medicaid |
|
On December 3, the Patient-Centered Outcomes Research Institute |
|
On November 23, HHS announced $35 million in funding for |
|
On November 12, CMS released a Preliminary Medicaid & |
|
On November 11, CMS finalized the Physician Fee Schedule |
|
On November 9, the FCC approved 75 new projects funded under the |
|
On October 15, HHS announced the renewal of the Public |
|
On August 26th, the FCC approved 62 new projects funded under the | The projects total $41.98 million for Round 2 of the COVID-19 |
On August 18, the Biden Administration invested over $19M to expand telehealth | The Biden Administration announced a series of key investments
Telehealth Centers of Excellence (COE) Program: |
On July 23rd, the Centers for Medicare and Medicaid Services | CMS is proposing to:
For more information regarding the Final CY2022 Physician |
On July 19th, HHS announced the renewal of the Public | The COVID-19 PHE will be renewed for another 90 days, beginning This update enumerates the key regulatory flexibilities and |
On June 17th, the Federal Communications Commission (FCC) |
|
On May 26th, the Department of Justice (DOJ) announced several criminal charges for |
|
On May 11th, the U.S. Department of Health & Human Services |
|
On May 6th, the Centers for Medicare & Medicaid Services |
|
On May 20th, the U.S. Department of Health & Human Services |
|
On May 19th the Government Accountability Office (GAO) released Medicare and Medicaid COVID-19 |
|
On April 15th the Federal Communications Commission | Appropriated by the Consolidated Appropriations Act, the $250 In an effort to promote transparency on how the funds are |
On April 12th the FDA lifted restrictions on telehealth | Healthcare providers will be allowed to prescribe |
On April 12th, HHS announced the Rural Maternity and | The $12 million program will fund three projects over four years One of the focus areas for the program includes telehealth and |
On April 5th, the U.S. Department of Agriculture (USDA) | The program makes $44.5 million available to helps rural Awards can range from $50,000 to $1 million. Applications must be received by June 4, 2021. |
On March 30th, the Centers for Medicare & Medicaid Services | CMS added several audiology and speech-language pathology |
On February 26th, HHS Office of the Inspector General (OIG) | OIG clarified in a letter the difference between ‘telefraud’ and ‘telehealth fraud’. Nothing that |
On February 25th, the USDA announced it is investing $42.3 million | USDA announced an investment of $42.3 million ($24 million |
On February 25th, the FCC approved the Emergency Broadband Benefit. | The FCC approved a new program which will provide discounts of The start date for the program has not yet been established. |
On January 19th, HHS’ OIG released an updated list of its Active Work Plan | HHS OIG announced it is conducting the Audit of Home Health |
On January 15th, the FCC announced the first round of grants for | The FCC has awarded a total of $26.6 million to 15 pilot |
On January 15th, CMS released a Preliminary Medicaid & CHIP Data | It includes information on services delivered from the beginning |
On January 12th, HHS invested $8 million in a new Telehealth | $6.5 million was awarded to the National Telehealth Technology The program is aimed at expanding broadband connectivity in |
On December 29th, the Department of Labor’s Wage and Hour | Employees can permanently use telehealth to establish a serious The Wage and Hour Division (WHD) will consider telemedicine an “in-person” visit. |
On December 3rd, HHS issued an amendment to the Public Readiness and Preparedness (PREP) |
|
On December 1st, CMS finalized the Physician Fee Schedule Rule (previously Note: On January 19th, CMS published clarifications to its 2021 Physician fee | Initial Rule: CMS finalized several changes to Prior to the PHE, given statutory restrictions that telehealth In addition to the changes to the telehealth covered services On a temporary basis, CMS finalized a policy to allow for CMS finalized as proposed several changes to coverage In addition, Medicare Diabetes and Prevention Program (MDPP) January 2021 Update: Clarifies that the Additionally, only one practitioner can bill CPT codes 99453 and For more information regarding the Final CY2021 Physician |
On November 20th, HHS published two rules that finalize reforms to the | HHS’s newly finalized regulations remove historical barriers Specifically, the regulations include several new and modified “safe harbor” arrangements that would allow providers and If a given arrangement meets all the criteria for a safe harbor, For more information regarding the Anti-Kickback and Stark Reforms, please see our Manatt Insights summary. |
In early November, CMS published a new final rule that enables health home | Services provided to patients must be included in the plan of |
On October 14, CMS expanded the list of telehealth services Medicare | CMS added 11 new services to the Medicare telehealth service |
On October 14, CMS released a Preliminary Medicaid and CHIP Data Snapshot to | This data shows more than 34.5 million services were delivered |
On August 4th, CMS released a proposed Physician Fee Schedule Rule which would | For CY 2021, CMS is proposing several changes to the Medicare For a summary of the proposed Physician Fee schedule Rule, |
On May 1, CMS released a second IFR with comment period (IFC), “Medicare and Medicaid Programs, Basic Health Program, and |
For a summary of the second IFR, please see the |
On April 17, CMS released Frequently Asked Questions (FAQs) on Medicare | New Payment for Telehealth Services (real-time, audio
Expansion of Virtual Communication Services (telephone, online
For more information on Expanded Telehealth Reimbursement |
On April 2, CMS issued an informational bulletin regarding Medicaid | This guidance provides states options for federal reimbursement For a summary of this bulletin, please see the April 6 Manatt Insights |
On March 30, CMS released an interim final rule (IFR) outlining new | These provisions include adding over 80 additional eligible For more information on the IFR, see our April 9 Manatt newsletter. |
On March 18, the HHS and the Office for Civil Rights (OCR) | This will allow providers to communicate with patients through For more information on our HIPAA summary, see our April 23 Manatt newsletter. |
On March 10, CMS introduced significant new | MA plans are required to:
For more information on Medicare changes, see our |
Legislative Activity
| Bill/Activity | Key Proposed Actions |
|---|---|
| Activity | |
In March 2021, MedPAC issued a report entitled “Medicare | The report included a chapter that proposes how Medicare may
After the PHE ends, MedPAC proposes: 1) returning to the fee
Notably, the path forward proposed by MedPAC in this report does |
On March 5th, the House Energy & Commerce Health | Members of the sub-committee were not aligned on a timeline for |
On January 14th, MedPAC hosted a meeting to discuss whether and | The Commissioners largely supported the policy options outlined The policy options will be incorporated into MedPAC’s For more information regarding the MedPAC meeting, please |
On November 9, MedPac issued a report on the expansion of | The presentation highlights permanent (post-PHE) policy options For more information, please see our Manatt Newsletter. |
| Introduced Legislation | |
Introduced September 27, 2022 |
|
Introduced September 22, 2022 |
|
S. 4747: Investing in Kids’ Mental Introduced August 2, 2022 |
|
HR.R. 8650 / S. 4723: Let Doctors Provide Reproductive Introduced August 2, 2022 |
|
Introduced July 28, 2022 |
|
H.R. 4040: Advancing Telehealth Beyond Engrossed July 27, 2022 |
|
H.R. 8489: Greater Access to Telehealth Introduced July 26, 2022 |
|
H.R. 8506: To amend title XVIII of the Introduced July 26, 2022 |
|
H.R. 8505: To amend title XVIII of the Introduced July 26, 2022 |
|
H.R. 8515: To amend title XVIII of the Introduced July 26, 2022 |
|
H.R. 8493: To amend title XVIII of the Introduced July 26, 2022 |
|
H.R. 8491:To amend title XVIII of the Social Introduced July 26, 2022 |
|
H.R. 8497: To amend title XVIII of the Introduced July 26, 2022 |
|
H.R. 8405 / S. 4467: Protecting Access to Medication H.R. 8405 Introduced July 18, 2022 S.4467 Introduced June 23, 2022 |
|
H.R. 8296: Women’s Health Protection Engrossed July 15, 2022 |
|
H.R.7900: National Defense Authorization Engrossed July 14, 2022 |
|
S. 2938: Bipartisan Safer Communities Passed June 25, 2022 |
|
S. 4498: Kids’ Mental Health Introduced June 23, 2022 |
|
S. 4486: Health Equity and Accountability Act Introduced June 23, 2022 |
|
H.R. 8169: Rural Telehealth Access Task Introduced June 22, 2022 |
|
H.R. 8180: Undertaking Needed Investments Introduced June 22, 2022 |
|
Introduced May 24, 2022 |
|
Introduced May 24, 2022 |
|
H.R. 7666: Restoring Hope for Mental Introduced May 6, 2022 |
|
H.R. 7585: Health Equity and Introduced April 26, 2022 |
|
H.R. 7573: Telehealth Extension and Introduced April 26, 2022 |
|
S. 4132: Women’s Health Protection Introduced May 4, 2022 (Note: Failed to pass the Senate on May 11, 2022) |
|
H.R. 7097: Telehealth Treatment and Technology Introduced on March 16, 2022 |
|
Introduced Feb. 8 2022 |
|
Telehealth Extension and Evaluation Act Introduced on Feb. 7, 2022 |
|
S. 150: Ensuring Parity in MA for Audio-Only Reintroduced Feb. 2, 2021 |
|
S. 155: Equal Access to Care Act Reintroduced Feb. 2, 2021 |
|
S. 340: Telehealth Response for E-prescribing Reintroduced Feb. 22, 2021 |
|
S. 368: Telehealth Modernization Act Reintroduced Feb. 23, 2021 |
|
S. 445: Mainstreaming Addiction Treatment Act Reintroduced Feb. 25, 2021 |
|
S. 620: KEEP Telehealth Options Act of Reintroduced Mar. 9, 2021 |
|
S. 660: Tele-Mental Health Improvement Act Introduced March 10, 2021 |
|
S. 801: Connected MOM Act Introduced Mar. 17, 2021 |
|
S. 1309: Home Health Emergency Access to Introduced Apr. 28, 2021 |
|
S. 1704/H.R.5981: Telehealth Expansion Act S. 1704 introduced May 19, 2021 H.R. 5981 introduced November 15, 2021 |
|
S. 2061: Telemental Healthcare Access Act of Introduced June 15, 2021 |
|
S. 2097: Telehealth Health Savings Account Introduced June 17, 2021 |
|
S. 2110: Increasing Rural Telehealth Access Introduced June 17, 2021 |
|
S. 2111: Audio-Only Telehealth for Emergencies Introduced June 17, 2021 |
|
S. 2173: Promoting Responsible and Effective Reintroduced June 22, 2021 |
|
S. 2197: Rural and Fronteir Telehealth Introduced June 23, 2021 |
|
H.R. 318: Safe Testing at Residence Telehealth Reintroduced Jan. 13, 2021 |
|
H.R. 341: Ensuring Telehealth Expansion Act of Reintroduced Jan. 15, 2021 |
|
H.R. 366: Protecting Access to Post-COVID-19 Reintroduced Jan. 19, 2021 |
|
H.R. 596: The Advancing Connectivity During Reintroduced Jan. 28, 2021 |
|
H.R. 708: Temporary Reciprocity to Ensure Reintroduced Jan. 19, 2021 |
|
H.R. 726: COVID–19 Testing, Reaching, Introduced Feb. 2, 2021 |
|
H.R. 937: Tech To Save Moms Act Introduced Feb. 8, 2021 |
|
H.R. 1149: Creating Opportunities Now for |
|
H.R. 1406: COVID-19 Emergency Telehealth Reintroduced Feb. 26, 2021 |
|
H.R. 1397: Telehealth Improvement for Kids’ Reintroduced Feb. 26, 2021 |
|
H.R. 2166: Ensuring Parity in MA and PACE for Bill text not yet available at the time of publication. |
|
H.R. 2168: Expanded Telehealth Access Act Bill text not yet available at the time of publication. |
|
H.R. 2228: Rural Behavioral Health Access Bill text not yet available at the time of |
|
H.R. 2903: CONNECT for Health Act Introduced Apr. 28, 2021 |
|
H.R. 3371: Home Health Emergency Access to Reintroduced May 20, 2021 |
|
H.R. 3447: Permanency for Audio-Only Introduced May 20, 2021 |
|
H.R. 3755: Women’s Health Protection Act Reintroduced June 8, 2021 |
|
H.R. 4012: Expanding Access to Mental Health Bill text not yet available at the time of |
|
H.R. 4040: Advancing Telehealth Beyond Reintroduced June 22, 2021 |
|
H.R. 4036 Introduced June 22, 2021 |
|
H.R. 4058 S.2061: H.R. 4058 introduced June 22, 2021 |
|
H.R. 4437: HEALTH Act of 2021 Introduced July 16, 2021 |
|
Introduced July 16, 2021 |
|
H.R. 4670: Advanced Safe Testing at Introduced July 22, 2021 |
|
H.R. 4770: Evaluating Disparities and Outcomes Introduced July 28, 2021 | Requires the Secretary of HHS to conduct a study evaluating the |
H.R. 4918: Rural Telehealth Expansion Introduced Aug. 3, 2021 | Amends the Social Security Act to include store-and- forward |
H.R. 5248: Temporary Responders for Introduced Sept. 14, 2021 | Authorizes the HRSA Provider Bridge Program to:
|
H.R. 5425: Protecting Rural Telehealth Access Introduced Sept. 29, 2021 |
Allows the use of audio-only technology for certain telehealth |
| Passed Legislation | |
H.R. 6074: Coronavirus Preparedness and |
For more information on Medicare changes, see our |
H.R. 748: Coronavirus Aid, Relief, and |
For more information on the CARES Act, see our March 27 Manatt |
H.R. 133: Consolidated Appropriations Act, |
For more information on the Consolidated Appropriations Act, |
H.R. 1319: American Rescue Plan Act of |
|
Relevant Telehealth Data and Reports
In November 2022, CTeL published a
legislative memo that provides summary of active
congressional bills that address Remote Patient Monitoring (RPM)
services and devices. Most active RPM bills require government
agencies to conduct an evaluation of the devices, and report back
to Congress on its use and effectiveness. Other active RPM
legislation would provide grants to states of providers to initiate
pilot programs and expand RPM services.
In June 2022, FAIR published an article titled “In March 2022, Telehealth Utilization Fell
Nationally for Second Straight Month“. Telehealth
utilization, as measured by telehealth’s share of all medical
claim lines, fell nationally for the second straight month,
according to FAIR Health’s Monthly Telehealth Regional Tracker.
Researchers suggest the decline in telehealth use was due to an
ongoing reduction in the severity and prominence of COVID-19,
encouraging more patients to attend in-person visits. The article
also states that despite the decline in overall telehealth usage,
mental health conditions remain at the top of the list of
telehealth diagnoses.
In May 2022, The National Committee for Quality Assurance (NCQA)
released a report titled “The Future of Telehealth Roundtable,”
which highlights strategies that could help close care gaps as
telehealth usage continues to grow. In October 2021, NCQA hosted a
roundtable discussion to facilitate dialogue on the future of
telehealth delivery in a post-pandemic world; the three following
strategies were identified to promote equitable access in
telehealth delivery:
- Creating telehealth services that cater to personal patient
preferences and needs, as some individuals may face struggles due
to their primary language and socioeconomic status - Addressing regulatory barriers to access and changing
regulations to allow expanded provider eligibility for
licensure - Leveraging Telehealth and Digital Technologies to Promote
Equitable Care Delivery
The report suggests that as telehealth becomes the new “normal”, it is important to prevent inequitable gaps in
telehealth delivery.
In May 2022, JAMA Pediatrics published a research letter titled, “Association of Race and Socioeconomic Disadvantage
With Missed Telemedicine Visits for Pediatric Patients During the
COVID-19 Pandemic.” The letter highlights how pediatric
patients are more likely to miss telehealth visits if they are
low-income. Specifically, a higher probability of economic
disadvantage was associated with a greater likelihood of missing a
telehealth visit as compared to an in-person visit across racial
groups. Additionally, telehealth visits were associated with lower
no-show rates for future clinical appointments, but only for those
with lower economic disadvantage.
In May 2022, Health Affairs published a study titled, “Medicare Beneficiaries In Disadvantaged
Neighborhoods Increased Telemedicine Use During The COVID-19
Pandemic.” The study found that Medicare beneficiaries
living in disadvantaged areas had the greatest odds of expanded
telehealth utilization as a result of emergency federal
telemedicine coverage expansions during the COVID-19 pandemic.
However, odds of increased telehealth access dropped as age
increased.
In May 2022, Harvard Business Review released an article titled “The Telehealth Era Is Just Beginning,”
which explored the current landscape and evidence around
telehealth, and discussed future trends in telehealth utilization
and policy coming out of the COVID-19 pandemic. Using internal data
from Kaiser Permanente and Intermountain Healthcare, combined with
National Committee for Quality Assurance outcomes data and health
plan member satisfaction surveys, the authors outline five
opportunities that broader telehealth utilization could
provide:
- A reduction in expensive, unnecessary ER visits
- An improvement in timeliness and efficiency of specialty
care - Access to the best doctors
- A reversal of America’s chronic-disease crisis
- Mitigation of health care disparities
The report also suggested that further integration among care
team members and adoption of capitated payment models may expedite
the implementation of telehealth.
RAND Corporation released a report titled “Experiences of Health Centers in Implementing
Telehealth Visits for Underserved Patients During the COVID-19
Pandemic“, which evaluated the progress of FQHCs that
participated in the Connected Care Acceleration (CCA) initiative by
investigating changes in telehealth utilization and health center
staff experiences with implementation. The study found that
although overall visit volumes remained about the same from the
pre-pandemic to the pandemic study periods, the share of audio-only
and video visits dramatically increased during the pandemic, and
audio-only visits were the leading modality for primary and
behavioral health. The study recommends continued study of
telehealth trends, particularly regarding equitable access to
telehealth.
In March 2022, the American Medical Association released
their 2021 Telehealth Survey Report, which aimed to
gather insights on the experiences of current and expected future
use to inform ongoing telehealth research and advocacy, resource
development, and continued support for physicians, practices, and
health systems. Data was collected from individuals, state and
specialty medical organizations, and members of the American
Medical Association Telehealth Immersion Program. The survey
indicated that 85% of physicians currently use telehealth, and over
80% of patients said that they receive better access to care since
using telehealth. In addition, 54.2% of respondents indicated that
telehealth has improved the satisfaction of their work, and 44%
said that telehealth has lowered costs.
In March 2022, GAO published a report titled “CMS Should Assess Effect of Increased Telehealth
Use on Beneficiaries’ Quality of Care“, which examined
the use of telehealth among Medicaid beneficiaries before and
during the COVID-19 pandemic across six select states: Arizona,
California, Maine, Mississippi, Missouri, Tennessee. The report
also explored the states’ experiences with telehealth during
the pandemic, future plans for post-PHE telehealth coverage, and
CMS’ oversight of quality of care for services delivered via
telehealth. GAO found that five of the selected states delivered
32.5 million services via telehealth to approximately 4.9 million
beneficiaries between March 2020 and February 2021, up from 2.1
million services delivered to about 455,000 beneficiaries during
the same time period in the previous year. Notably, the report
highlighted the need for improved data collection and analysis
related to the quality of care delivered via telehealth. Based on
the results of the study, GAO issued two recommendations to CMS:
(1) collect and analyze information about the effect delivering
services via telehealth has on the quality of care Medicaid
beneficiaries receive, and (2) determine any next steps based on
the results of the analysis.
In March 2022, the HHS-OIG released a data brief titled “Telehealth Was Critical for Providing Services to
Medicare Beneficiaries During the First Year of the COVID-19
Pandemic,” which examined trends in telehealth utilization
among Medicare fee-for-service and Medicare Advantage beneficiaries
from March 2020 to February 2021. The data brief indicated that
more than 40% of Medicare beneficiaries utilized telehealth during
the first year of the pandemic, with use remaining high through
early 2021. Beneficiaries used 88 times more telehealth services
during the first year of the pandemic as compared to the prior
year.
In March 2022, the American Medical Association (AMA) released
a physician survey examining experiences
with and perceptions of telehealth. Of the 2,232 provider
respondents, nearly 85% indicated they currently use telehealth to
deliver care to patients, while 70% indicated they plan to continue
offering telehealth services. Moreover, 60% of providers surveyed
felt telehealth enabled them to provide high quality care, while
80% of respondents indicated patients received better access to
care since using telehealth.
In February 2022, the American Medical Association (AMA), in
collaboration with Manatt Health, published a report titled “Accelerating and Enhancing Behavioral Health
Integration Through Digitally Enabled Care,” which used
findings from a diverse working group to highlight solutions that
industry stakeholders can apply to address gaps hindering the
equitable and sustainable adoption of digitally-enabled behavioral
health integration (BHI). Solutions included: increasing BHI
training for primary care and behavioral health providers through
the incorporation of digitally enabled BHI into standard curricula,
encouraging the incorporation of telehealth into BHI by
implementing payment parity for behavioral health services
delivered via video or audio-only modalities, and passing
legislation to remove originating site and geographic restrictions
for all telehealth services in Medicare that limit access to
care.
In February 2022, Doximity, a provider networking and digital
health service, published the second edition of its “State of Telemedicine Report,” which
highlighted findings in patient and provider perceptions of
telehealth based on surveys conducted between January 2020 and June
2021. Patients overall showed growing trust in telehealth as a
mechanism for high-quality care, with 55% reporting that they felt
telemedicine provided equal or greater quality of care than
in-person visits in 2021, compared to 40% in 2020. In addition,
approximately two thirds of physicians indicated that using
telemedicine allowed them to build or preserve trust with their
patients.
In February 2022, The U.S. Government Accountability Office
(GAO) released a report titled, “Defense Health Care: DOD Expanded Telehealth for
Mental Health Care during the COVID-19 Pandemic,” which
focused on telehealth use in the military. Among active duty
servicemembers, pre-pandemic telehealth visits made up 15% of
mental health care visits, compared to 33% in April 2021.
Department of Defense (DOD) officials highlighted the value of
telehealth and its ability to improve access and continuity of
care. In addition, officials suggested that telehealth may reduce
the stigma of seeking mental health treatment by allowing
servicemembers to receive care more privately without the risk of
being seen in military treatment facilities.
In February 2022, the HHS Office of the Assistant Secretary for
Planning and Evaluation released an issue brief titled “National Survey Trends in Telehealth Use in 2021: Disparities
in Utilization and Audio vs. Video Services,” which compared
differences in telehealth access for audio-only and video visits
between April and October 2021. While overall telehealth
utilization was similar across demographic groups, except among the
uninsured, there were significant differences in video telehealth
use. Rates of video telehealth use were lowest among Latino, Asian
and Black individuals, those without a high school degree and
adults ages 65 and older.
In October 2021, the HHS-OIG released a data snapshot report
titled “Most Medicare beneficiaries received telehealth
services only from providers with whom they had an established
relationship,” which evaluated the relationship between
providers and Medicare patients utilizing telehealth between March
and December 2020. Notably, the data snapshot found that 84% of
Medicare beneficiaries received telehealth services only from
providers with whom they had an established relationship.
In October 2021, JAMA published an study titled “Changes in
Virtual and In-Person Health Care Utilization in a Large Health
System During the COVID-19 Pandemic,” which sought to assess
the association between the growth of virtual care and health care
utilization in an integrated delivery network. The study found that
while COVID-19 caused in-person visits to decline and virtual
services to increase, there was no significant change in the
overall volume of healthcare utilization, suggesting that virtual
care was substitutive, rather than additive in the ambulatory care
setting.
In September 2021, the HHS-OIG released two telehealth reports “States Reported Multiple Challenges With Using
Telehealth To Provide Behavioral Health Services to Medicaid
Enrollees” and “Opportunities Exist To Strengthen Evaluation and
Oversight of Telehealth for Behavioral Health in Medicaid”
based on surveys conducted in early 2020. The surveys focused
around telemental health delivery though managed care
organizations.
In July 2021, AAMC in in partnership with Manatt Health
published “Sustaining Telehealth Success: Integration
Imperatives and Best Practices for Advancing Telehealth in Academic
Health Systems“, conducting extensive interviews with many
leading telehealth AMCs across the country (Ochsner, VA, Kaiser,
MUSC, UMMC, Intermountain, Jefferson, etc.) and synthesizing best
practices through this report.
In July 2021, The National Association of Community Health
Centers (NACHC) published “Telehealth During COVID-19 Ensured Patients Were
Not Left Behind,” which explores how health centers have
utilized telehealth and the implications for health center patients
should the PHE flexibilities not be extended.
In June 2021, the Lucile Packard foundation published “COVID-19 Policy Flexibilities Affecting
Children and Youth with Special Health Care Needs” to
identify key flexibilities enacted during the PHE related to
children and youth with special health care needs (CYSHCN) and
summarize stakeholders’ perspectives about the impact of policy
flexibilities on CYSHCN and their families and providers.
In June 2021, the Commonwealth Fund published “States’ Actions to Expand Telemedicine Access
During COVID-19 and Future Policy Considerations,” which
examined state actions to expand individual and group health
insurance coverage of telemedicine between March 2020 and March
2021 in order to better understand the changing regulatory approach
to telemedicine in response to COVID-19.. Notably, the report found
that twenty-two states “changed laws or policies during the
pandemic to require more robust insurance coverage of
telemedicine.” Three policy flexibilities that states focused
on included: requiring coverage of audio-only services; requiring
payment parity between in-person and telemedicine services; and,
waiving cost sharing for telemedicine or requiring cost sharing
equal to in-person care.
In June 2021, the Substance Abuse and Mental Health and Services
Administration (SAMHSA) released “Telehealth for the Treatment of Serious Mental
Illness and Substance Use Disorders,” a guide supporting
the implementation of telehealth across diverse mental health and
substance use disorder treatment settings. The guide examines the
current telehealth landscape and includes guidance and resources
for evaluating and implementing best practices that will continue
to assist treatment providers and organizations seeking to increase
access to mental health services via telehealth.
In May 2021, the National Academy for State Health Policy
(NASHP) released “States Expand Medicaid Reimbursement of
School-Based Telehealth Services” exploring how states are
increasing Medicaid coverage of school-based telehealth services
during COVID-19, determining which services can effectively be
delivered through telehealth, and supporting equitable access to
telehealth services for students.
In May 2021, the Kaiser Family Foundation published “Medicare and Telehealth: Coverage and Use During
the COVID-19 Pandemic and Options for the Future”
analyzing Medicare beneficiaries’ utilization of telehealth
using CMS survey data between summer and fall of 2020.
In May 2021, the American Medical Association in partnership
with Manatt Health published “Return on Health: Moving Beyond Dollars and Cents
in Realizing the Value of Virtual Care” to articulate the
value of digitally enabled care that accounts for ways in which a
wide range of virtual care programs can increase the overall health
and generate positive impact for patients, clinicians, payors and
society.
In March 2021, the Journal of the American Medical Association
(JAMA) published “In-Person and Telehealth Ambulatory Contacts
and Costs in a Large US Insured Cohort Before and During the
COVID-19 Pandemic,” highlighting existing disparities related
to the digital divide.
FAIR Health publishes a Monthly Telehealth Regional Tracker to
track how telehealth is evolving comparing telehealth: volume of
claim lines, urban versus rural usage, the top five procedure
codes, and the top five diagnoses.
In February 2021, the Commonwealth Fund published “The Impact of COVID-19 on Outpatient Visits in
2020: Visits Remained Stable, Despite a Late Surge in
Cases” tracking trends in outpatient visit volume through
the end of 2020 hoping to track what the clinical impacts of the
pandemic are and how accessible has outpatient care been, if there
are new policies encouraging greater use of telemedicine, and what
has been the financial impact of the pandemic on health care
providers.
In February 2021, the California Health Care Foundation in
partnership with Manatt Health published “Technology Innovation in Medicaid:What to Expect
in the Next Decade,” a survey of 200 health care thought
leaders in order to learn where health technology in the safety net
is expected to go over the next decade.
In February 2021, Health Affairs published “Variation In Telemedicine Use And Outpatient
Care During The COVID-19 Pandemic In The United States”,
which examined outpatient and telemedicine visits across different
patient demographics, specialties, and conditions between January
and June 2020. The study found that 30.1% of all visits were
provided via telemedicine, and usage was lower in areas with higher
rates of poverty.
On December 29, JAMA published an article evaluating whether
inequities are present in telemedicine use during the COVID-19
pandemic. The study found that older patients, Asian patients, and
non–English-speaking patients had lower rates of telemedicine
use, and older patients, female patients, Black, Latinx, and poorer
patients had less video use. The authors conclude that there are
inequities that exist and the system must be intentionally designed
to mitigate inequity.
The content of this article is intended to provide a general
guide to the subject matter. Specialist advice should be sought
about your specific circumstances.
#Affordability, #Black, #Children, #Coronavirus, #CostSharing, #Coverage, #Employers, #Enrollment, #FamilyPlanning, #HealthCenters, #Hispanic, #Medicaid, #Medicare, #MentalHealth, #NursingFacilities, #PublicHealth, #Seniors, #Telehealth, #Uninsured, #Utilization
Published on The Perfect Enemy at https://bit.ly/3HnUdPl.
Comments
Post a Comment
Comments are moderated.